In the realm of pelvic health, urinary concerns often take the spotlight, leaving many surprised to discover the intricate involvement of the pelvic floor in bowel movement. This article aims to shed light on this lesser-discussed connection, exploring how pelvic floor dysfunctions can lead to both constipation and incontinence.
We will begin by explaining the different types of functional constipation. From there, we will delve into the mechanics of bowel control and its potential breakdown, giving rise to constipation and/or incontinence. By the end of this read, you will have a clear grasp of the inner workings of bowel movement physiology and gain insights to make informed choices for your pelvic health.
Let's quickly recall a few notions first. The rectum serves as the faeces storage unit. It is the last part of the large intestine (also called the colon), right before the anus. The ability to hold in your bowels is called continence. In contrast, incontinence is when you lose bowel control and have an accidental leakage.
Table of contents
- The differences between Transit and Outlet constipation
- Bowel Control 101
- Bowel Movement Process
- Non-relaxing pelvic floor
- Defective propulsion forces of the rectum
- Rectocele
- Avoid constipation at all costs
- Bowel Incontinence is one of the unexpected consequences of constipation
- It is never too late to start taking care of your pelvic health
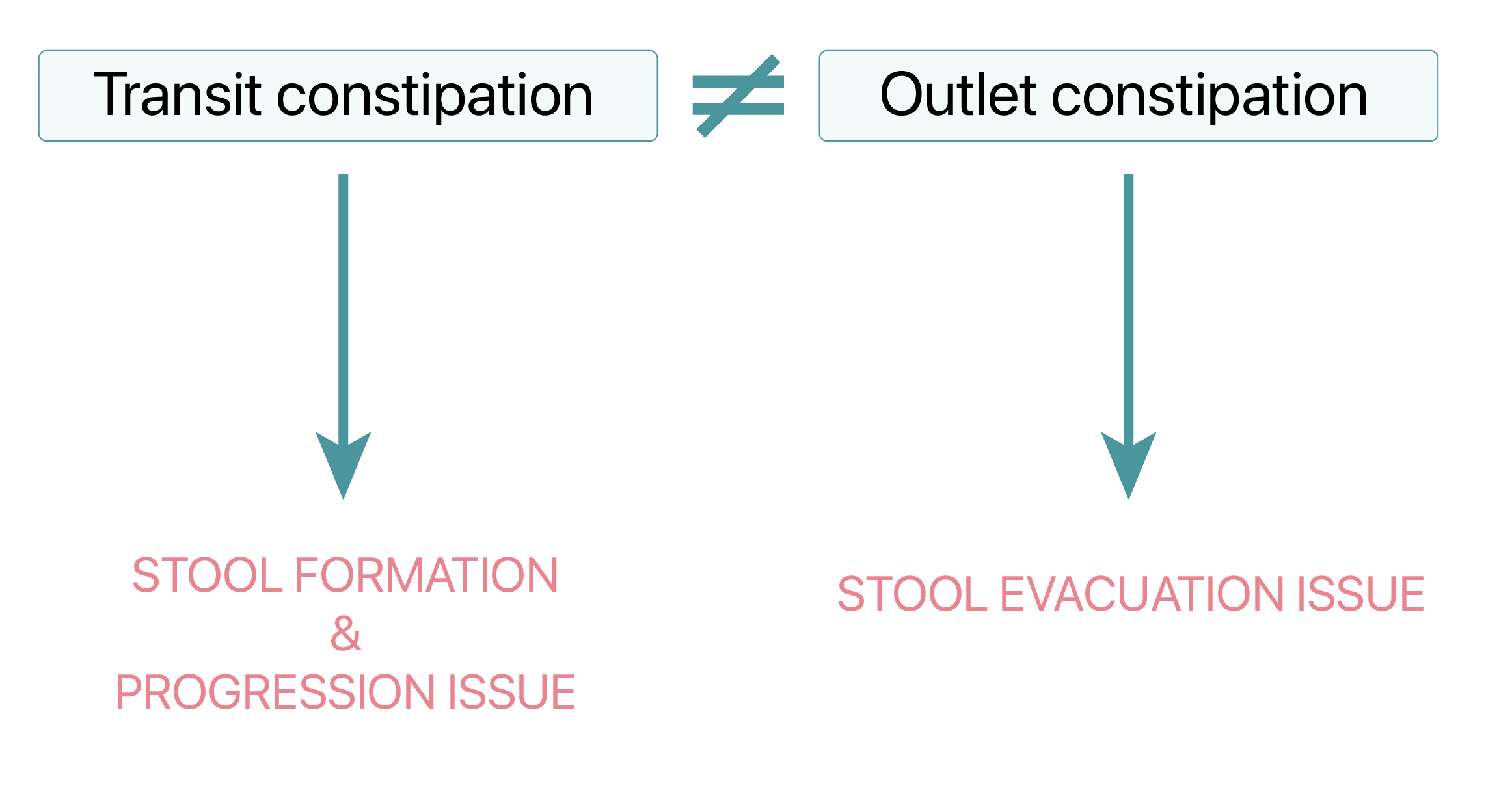
The differences between Transit and Outlet constipation
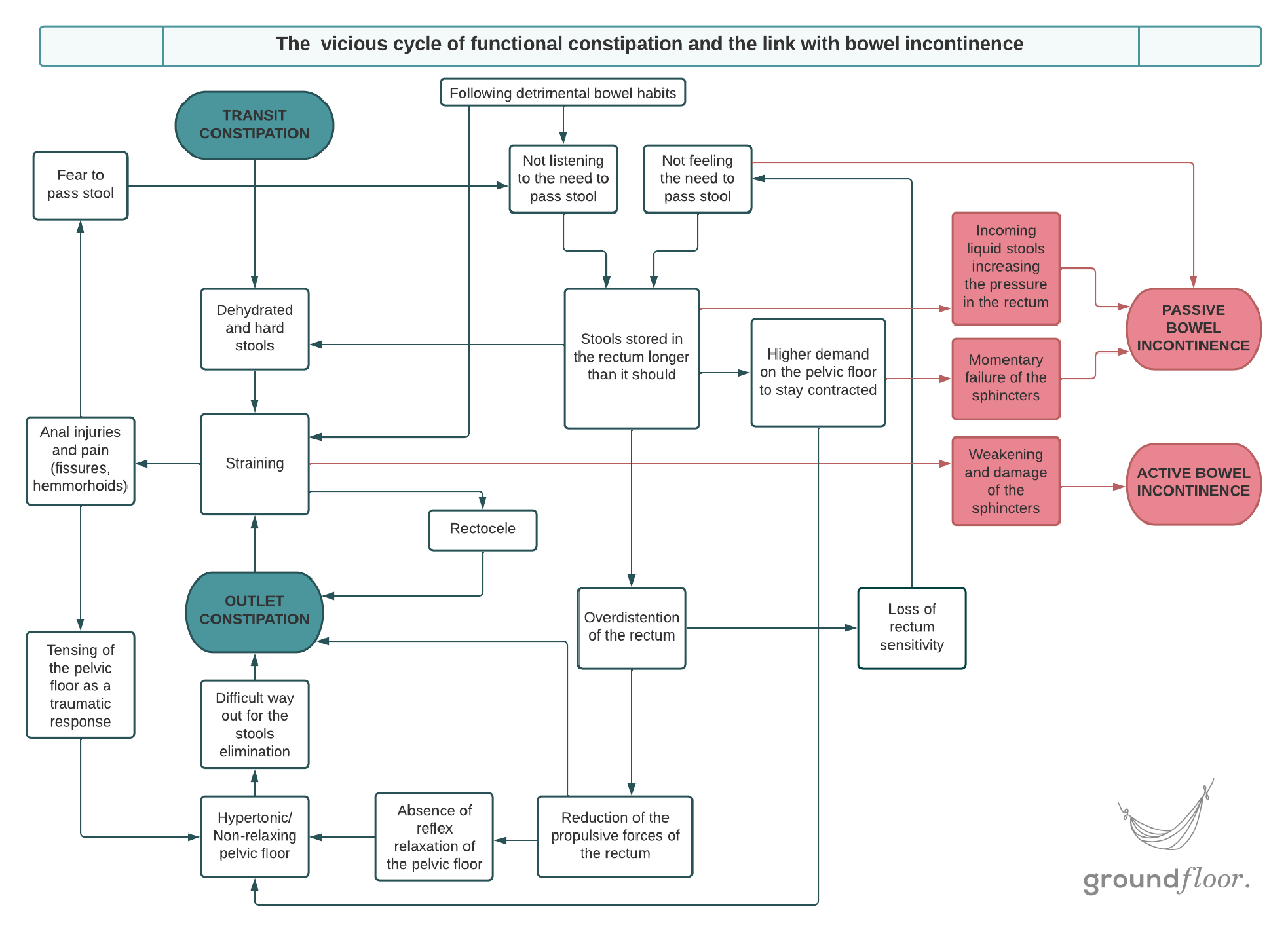
Most people only know about transit constipation. It typically occurs when the consistency and frequency of bowel movements are affected by dietary choices. It can also be caused by the process the food goes through in your digestive tract before it reaches its final destination, the rectum.
The pelvic floor and the rectum are the last functional elements of the digestive system. Outlet constipation, also called dyschezia or obstructive constipation, is when these two components fail to function together or separately, hindering a smooth and complete passage of stool. It is a "gate control" dysfunction, where the opening system that should enable bowel movement is malfunctioning.
Unfortunately, those two types of constipation often coexist simultaneously, requiring actions on both ends of the digestive process.
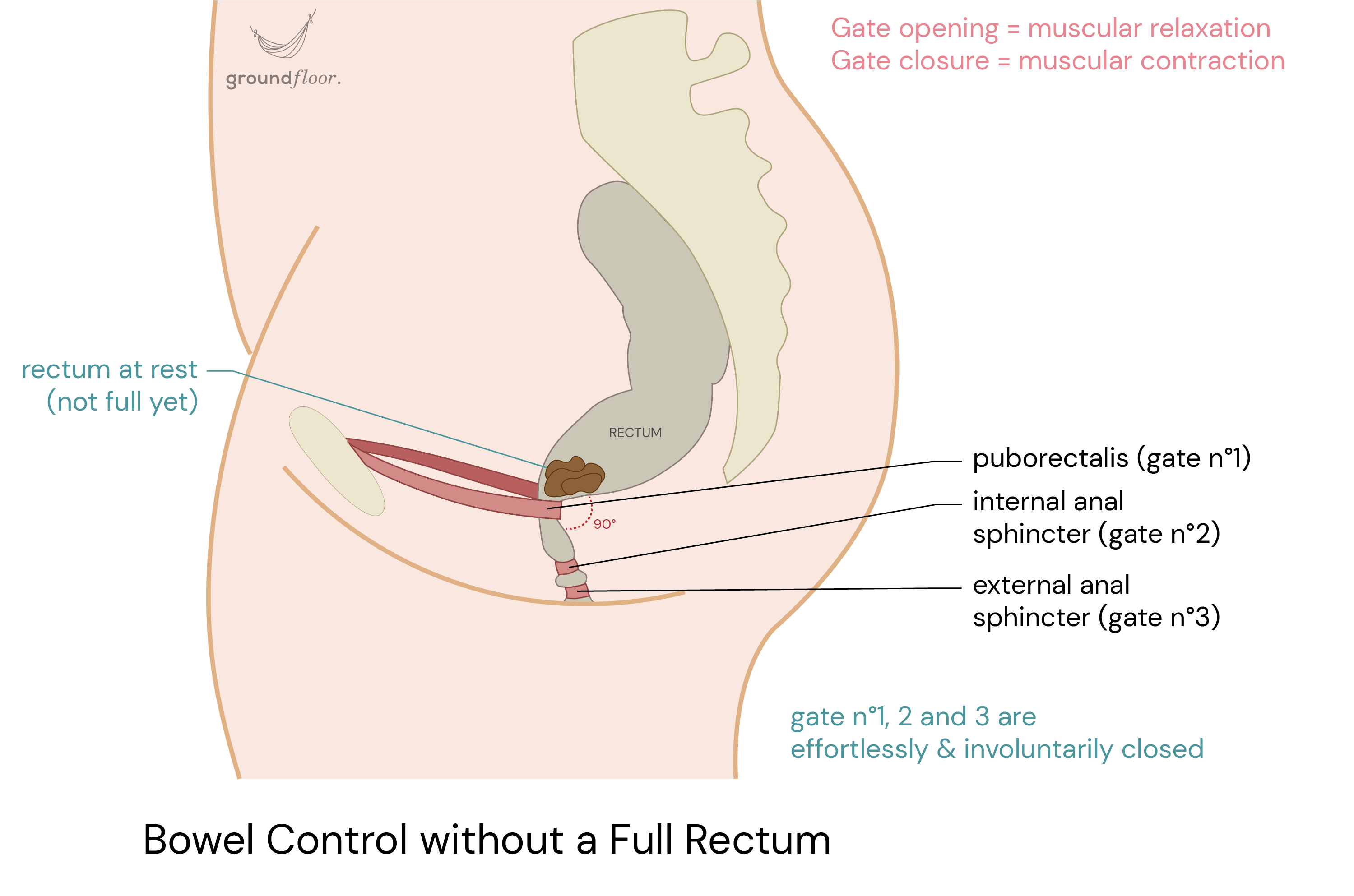
Bowel Control 101
Let's start by delving into the process that maintains continence and prevents accidental bowel leakage. It begins with the puborectalis (gate n°1), a sling attached to both ends of the pubic bone. It wraps around the rectum and pulls it forward, creating a 90° angle bend with the anal canal. This muscle is the first element of continence. It acts as a valve by forming an anatomical barrier that prevents the involuntary outflow of stool.
Two other pivotal muscles contribute to continence: the internal anal sphincter (gate n°2) and the external anal sphincter (gate n°3) located just below it. They both remain constantly activated without conscious effort, serving as sealed locks.
Bowel Movement Process
A cascade of events occurs to initiate the bowel movement process. In normal circumstances, once enough faeces have accumulated in the rectum, the rectal walls contract, propelling the stools downward and giving rise to the sensation of urge.
The puborectalis relaxes as a reflex, which widens the anorectal angle, producing a straight way out for faeces to exit.
The internal anal sphincter opens up only to follow the puborectalis relaxation when the rectum contracts and propels the stools.
In contrast, the external anal sphincter contracts even more robustly, creating an effective barrier to retaining stools. This stage empowers you to make a choice. You can either proceed to pass stools now (by relaxing the external sphincter to open the final gate) or hold longer (by maintaining the contraction of the last gate until the stools travel back up and the urge subsides).
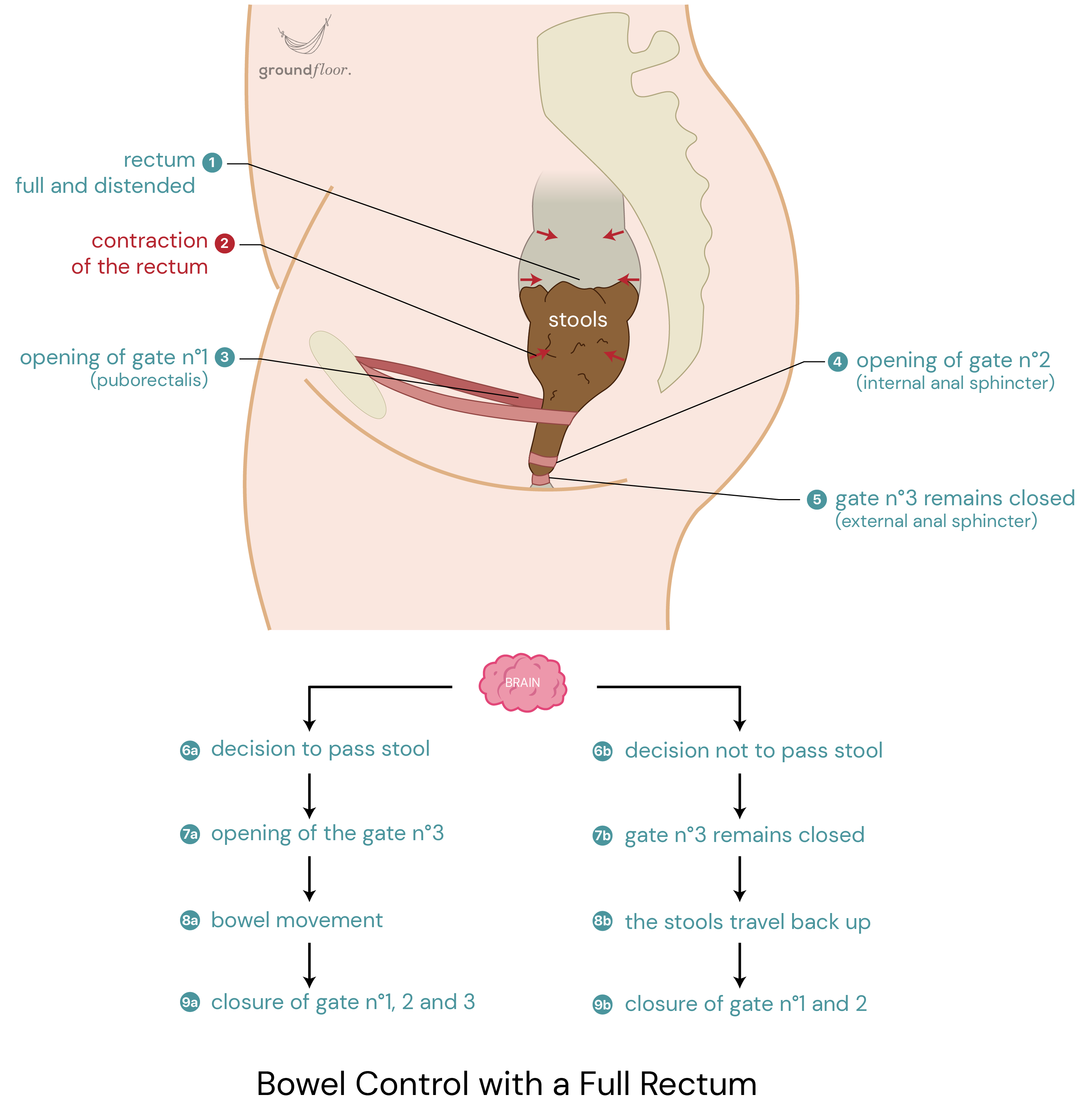
In the absence of dysfunction, there's no need to strain to have a bowel movement. It may occasionally be required as a "starter" only to initiate the mechanism described above. Under optimal circumstances, after feeling the urge to pass stools, sitting in the optimal defecation position and relaxing should be enough. The synchronized expulsive contractions of the rectum and the relaxation of the pelvic floor muscles (comprising the three "gates") enable effortless passage of stools, eliminating the need for effort or straining.
Outlet constipation occurs when something goes wrong in one or multiple steps of the bowel movement mechanism. In the following sections, we will outline the most common causes, which often accumulate and become self-sustaining...
Non-relaxing pelvic floor
A hypertonic pelvic floor is a common underlying cause of Outlet Constipation. When the puborectalis, internal, or external anal sphincters don't relax adequately, they obstruct the passage for stool elimination.
In some cases, individuals experience anismus, also known as paradoxical puborectalis syndrome or pelvic floor dyssynergia. This condition involves the puborectalis (gate n°1) contracting even stronger, creating a sharper anorectal angle during attempted defecation. This further tightens the passage for stools and prevents the automatic relaxation of the anal sphincters. As a result, the three "gates" remain firmly sealed, leaving no alternative but forceful and violent straining to pass stools, increasing the risk of injury. These attempts are often painful, prolonged, frustrating, and frequently fail.
Defective propulsion forces of the rectum
Outlet constipation can also result from ineffective contraction forces of the rectum, which impair the proper propulsion of stools. As described above, the subsequent cascade of events leading to bowel movement cannot occur efficiently without this step.
This dysfunction is often induced by the muscular walls becoming overdistended due to leaving stagnating faeces in the rectum for too long. Indeed, repetitively not answering the need for bowel movement is the onset of a vicious cycle. It gradually affects rectal sensitivity and diminishes the ability to recognize the urge for bowel movements. Consequently, passing stool becomes less frequent, further contributing to overloading and overstretching the rectum. This, in turn, leads to damage in the muscular rectal walls, reducing the ability to generate the necessary force for propelling bowel content.
The habit of not listening to our bowels on time exemplifies how our behaviour can negatively impact pelvic health in the long term.
Rectocele
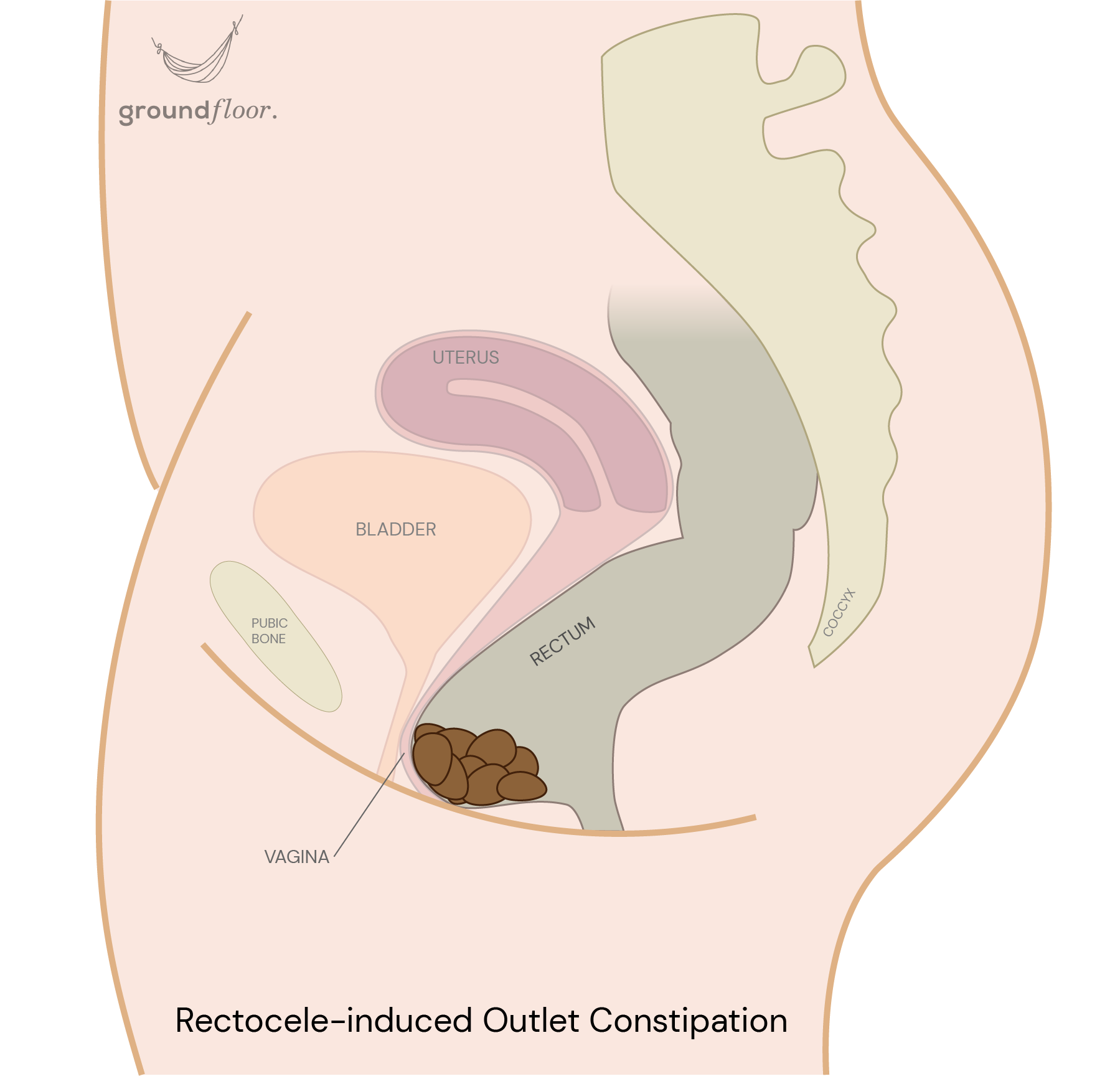
The last common cause of outlet constipation is the presence of a rectocele (rectal prolapse). Let's remind first that the vagina and the rectum are two cavities sharing a common wall. When the separation between both organs loses its upright shape, the rectum protrudes into the vagina, forming a pocket known as the rectocele, where stool can become trapped.
Individuals afflicted with this condition usually resort to straining while attempting to evacuate their bowels. Regrettably, straining is likely the root cause of this problem, compounding it over time. It worsens the rectocele by weakening and impairing the already compromised support system.
Avoid constipation at all costs
Irrespective of the type, always remember that constipation is the worse enemy of your pelvic floor. It places an undue burden on the pelvic system necessitating forceful straining during bowel movements. It inflicts an additional, unnecessary, and tremendous amount of pressure. Such excessive stress is overwhelming for your pelvic floor to bear day after day, especially if you have been afflicted by constipation for years.
Constipation often leads to injuries like haemorrhoids, anal fissures, and other complications, including urinary incontinence, prolapse, dyspareunia, and pudendal neuropathy, to name just a few. For example, the risk of an overactive bladder is multiplied by 2 or 4 with constipation compared to individuals without.
Bowel Incontinence is one of the unexpected consequences of constipation
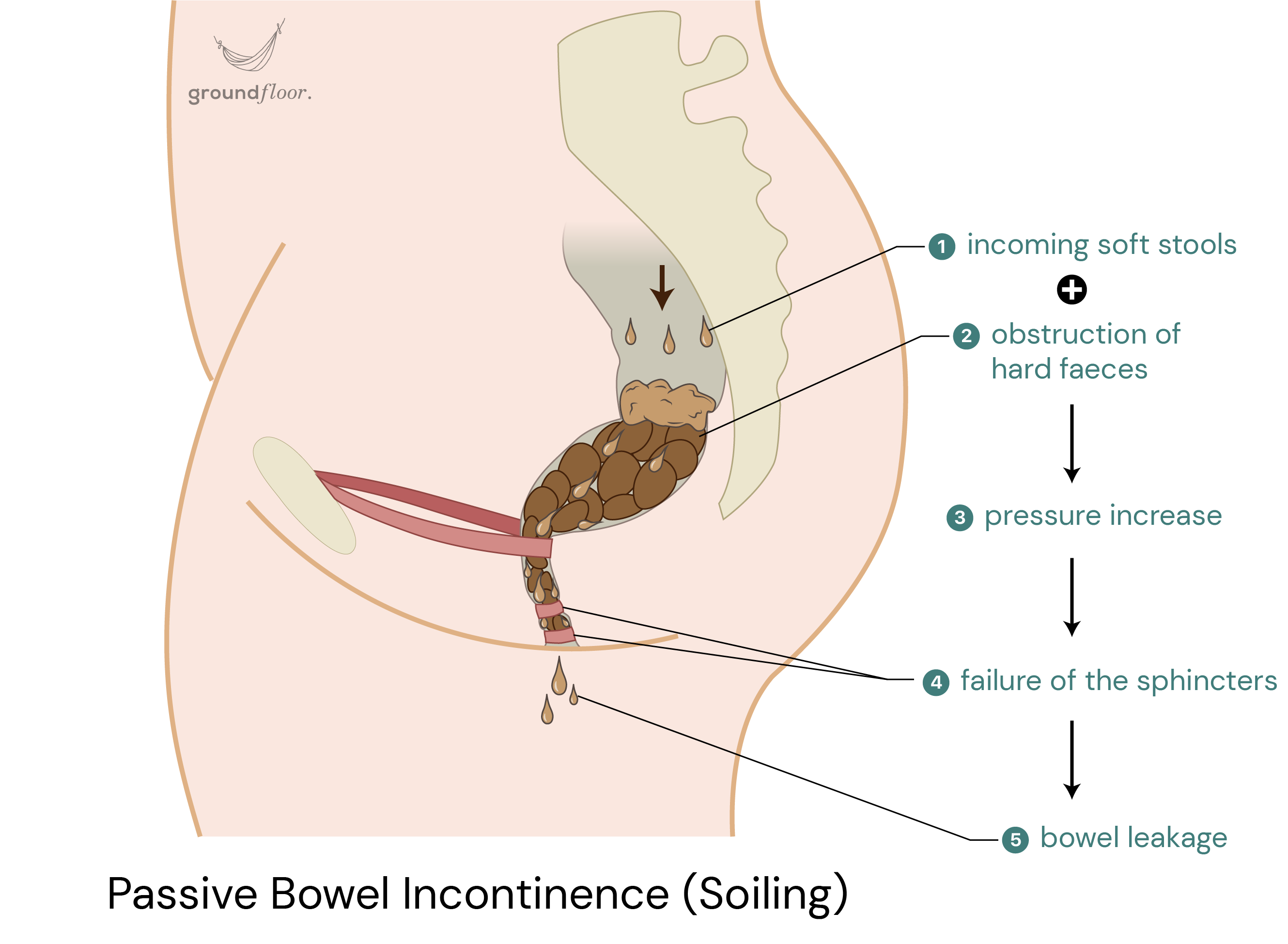
It might seem paradoxical, but constipation can also cause incontinence. Indeed, liquid stools can seep around hard faeces obstructing the rectum when the pressure builds up. Those in this situation often don't perceive the urge to have a bowel movement before experiencing leakage. It is called passive bowel incontinence or soiling.
In contrast, active bowel incontinence occurs when individuals feel the urge for bowel movement but cannot hold it until reaching the toilet in time. This issue arises from a defective, compromised, or weakened pelvic floor, which can't maintain the "gates" effectively closed. Unfortunately, repetitive episodes of constipation accompanied by straining elevate the risk of developing this problem over time by damaging the structural integrity of the pelvic floor.
In short, addressing constipation becomes a safeguard against both passive and active bowel incontinence in the short and long term. However, eliminating constipation is challenging as it is simultaneously the cause and the consequence of pelvic floor dysfunctions. It perpetuates a vicious cycle, where each stage paves the way for the next.
Indeed, pelvic floor issues often lead to one another, but it is particularly evident with chronic constipation. If you find yourself in this situation, you likely already have some pelvic floor dysfunctions you are unaware of. And it is probably just a matter of time before additional issues emerge…
It is never too late to start taking care of your pelvic health
Are you experiencing infrequent bowel movements? Hard stools? Uncomfortable or painful trips to the bathroom? Or even anal injuries? Have you ever had an accidental bowel leakage (even once)?
Take your check-up to discover how to get your bowel on the right track. Your tailored program will address your unique pelvic health concerns, whether your goal is to break free from the cycle of constipation, overcome incontinence, or address both issues.
Based on your individual needs, you can access the bowel training feature to help you establish a regular bowel movement rhythm, effectively targeting any challenges you might be facing with bowel control.
Certain behavioural adjustments might also be recommended to improve your situation and prevent future problems. The Bowel Care Guide and the Habits Tracker will guide you on necessary lifestyle changes and provide support to keep you on course. Additionally, following the analysis of your overall pelvic health through the check-up, specific pelvic floor exercises can be provided if deemed beneficial.
Share this article with your friends and help spread the knowledge together! ↓
Share this article with your friends and help spread the knowledge together! →





Download the app to learn more about this topic and receive tailored information about your pelvic health!


Related articles
7 min read
The truth about having a tight pelvic floorA hypertonic or overactive pelvic floor (distinct from an overactive bladder) results from the buildup of excessive tension within the muscles. In this situation, the pelvic floor can also be referred to as "tight", which is often wrongly believed to be a good thing. This article will debunk this myth and shed light on the misconceptions surrounding this topic. Delving into the consequences of such a condition, we will also explore the common errors that can lead to a hypertonic pelvic floor and provide effective and practical strategies to address it.
→ Read more
4 min read
How pelvic floor training protects you from incontinenceDiscover your pelvic floor's vital role in maintaining bladder and bowel control. Learn how to care for it effectively to prevent unintentional leakage. This article will explore the mechanisms behind continence, define incontinence, highlight its impact on women's lives, and emphasise the importance of targeted solutions.
→ Read more
3 min read
Turn on the automatic mode of your pelvic floorYou may have been training your pelvic floor wrong this whole time! One-size-fits-all exercises can't unlock the full potential of your pelvic floor. This article will discuss why tailoring your training is crucial to target your specific needs. You will also learn about the Knack, the alternative to doing Kegels forever, that will make your pelvic floor work automatically!
→ Read more

