Discover the vital importance of the pelvic floor's support function, a topic often neglected but essential for optimal pelvic health. This article will give you insights into caring for your pelvic floor, effectively preventing problems associated with an impaired support system. Armed with this knowledge, you can proactively reduce the risk of issues such as pelvic organ prolapse and perineum descent.
Table of contents
- The support role of the pelvic floor
- The consequences of a dysfunctional pelvic support
- The role of a functional pelvic floor musculature for an effective support system
- Protecting passive pelvic floor structures for effective support
- The consequences of intra-abdominal pressure on the support system
- The consequences of a hypertonic pelvic floor on the support system
The support role of the pelvic floor
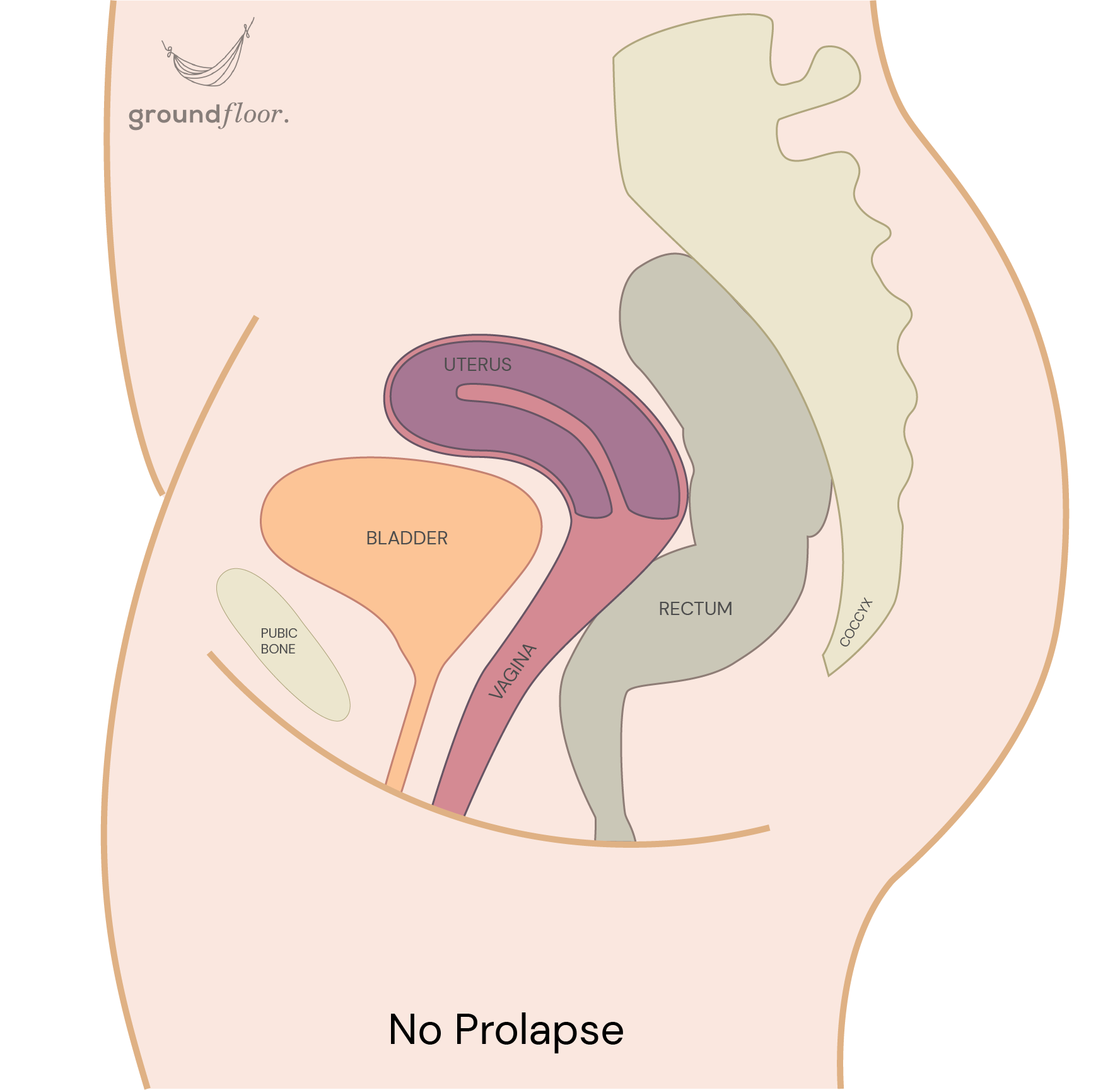
One of the primary functions of the pelvic floor is supporting the bladder, uterus, and rectum. This anatomical structure constitutes the bottom of the abdominal cavity, upon which all forces within the trunk are directed onto. Hence the name "floor"! Due to its position within the body, gravity also exerts a downward force on it when in an upright position.
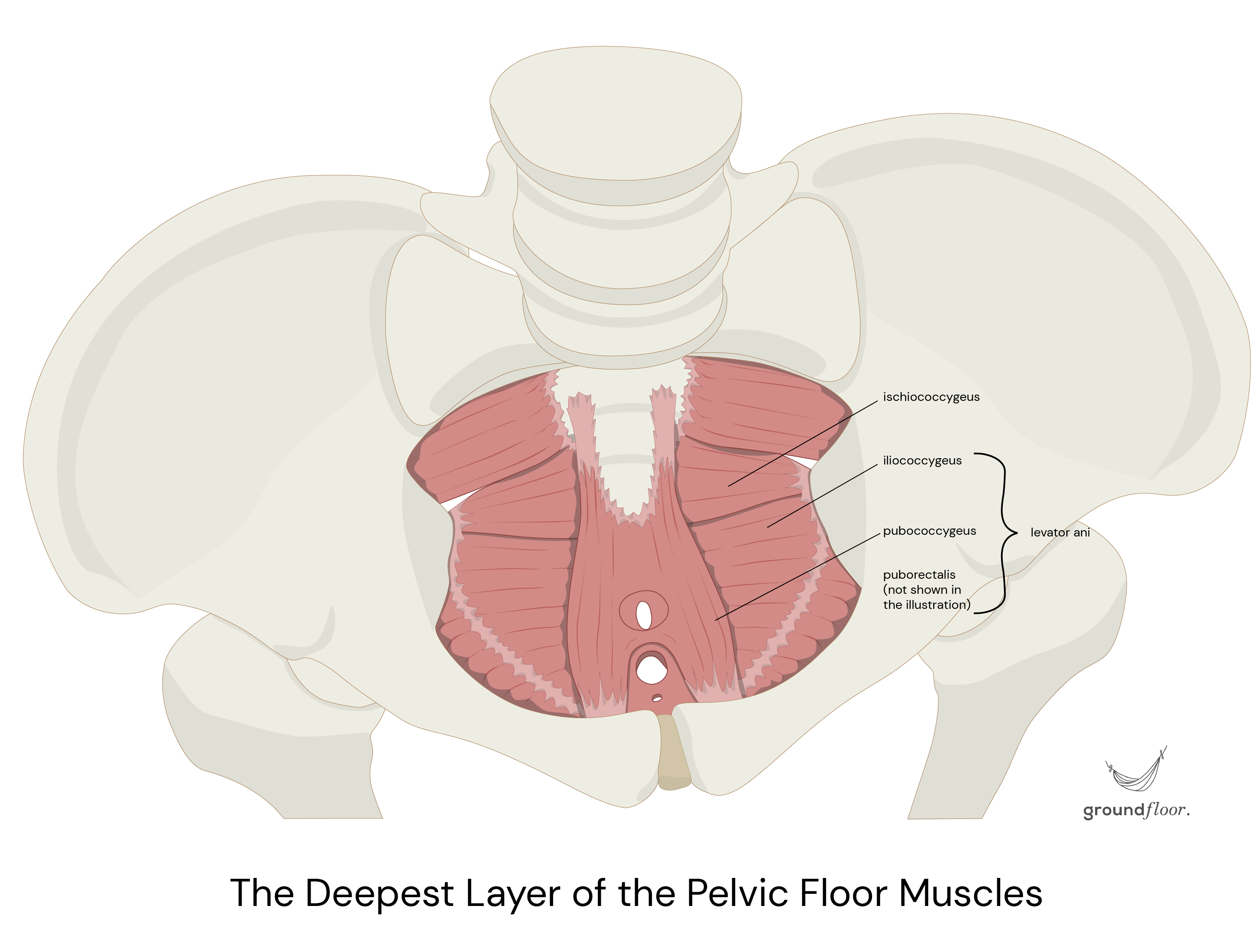
Let's quickly recall that the deepest layer of the pelvic floor muscles (the ischiococcygeus and levator ani) forms a hammock-like structure. It spans from the pubic bone to the tailbone (front to back) and extends between both sit bones (side to side).
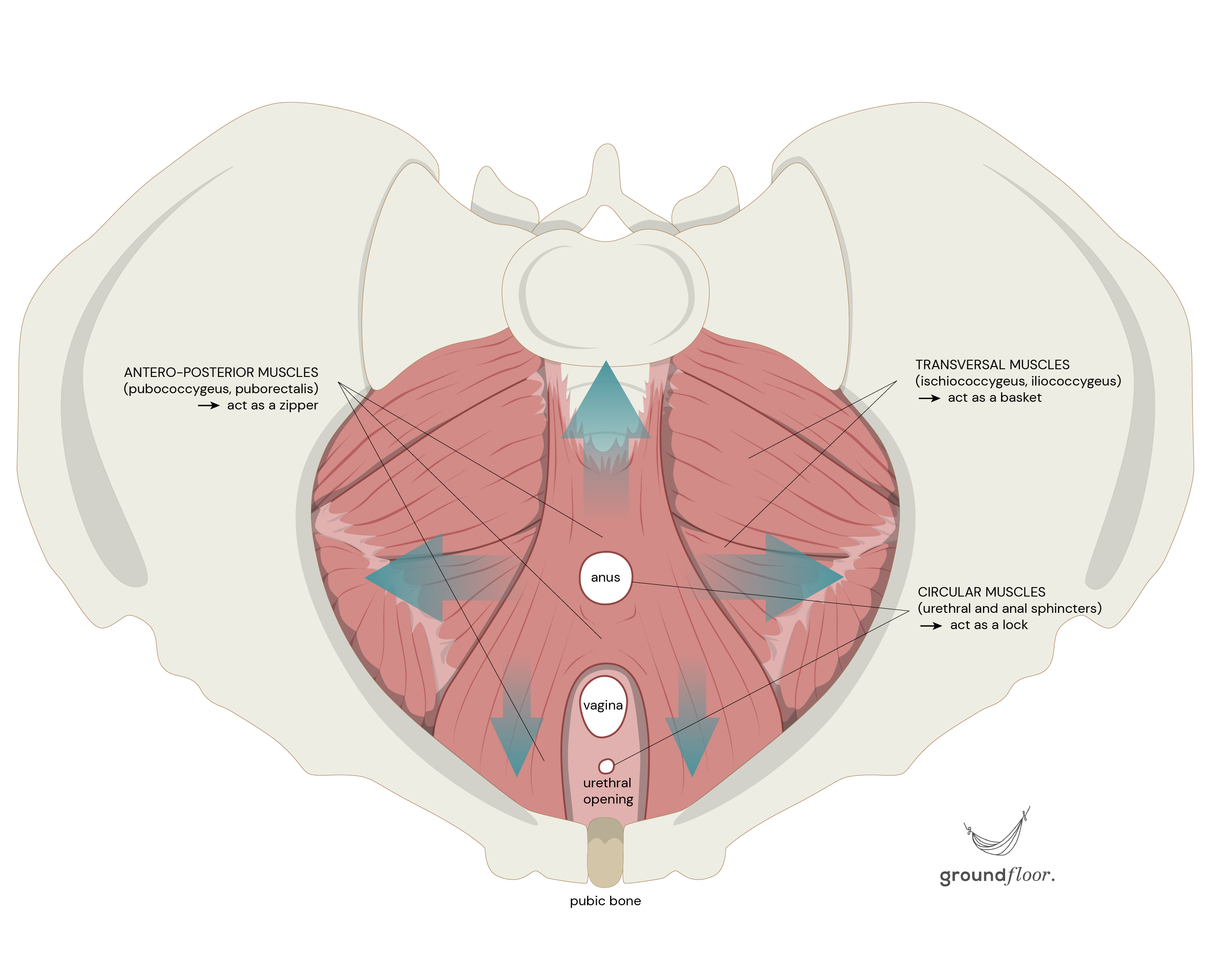
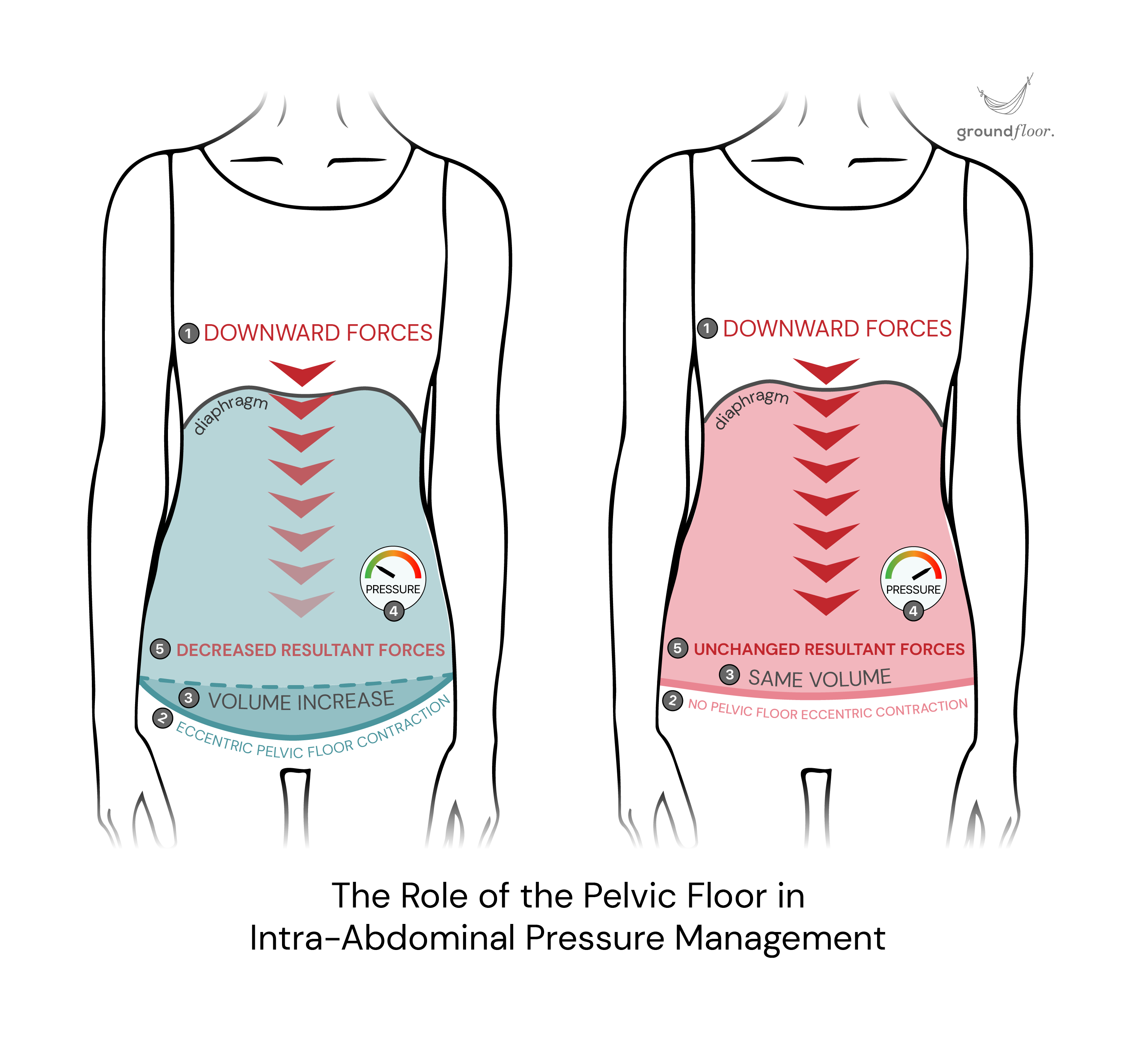
The pelvic floor muscles contract to achieve closure of the sphincters and counteract the downward pressure caused by increased pressure in the abdominal cavity (trunk). It happens in situations like sneezing, coughing, straining, lifting, running, etc. The strength of the contraction must be adapted to the level of strain in action to effectively hold the pelvic organs where they belong.
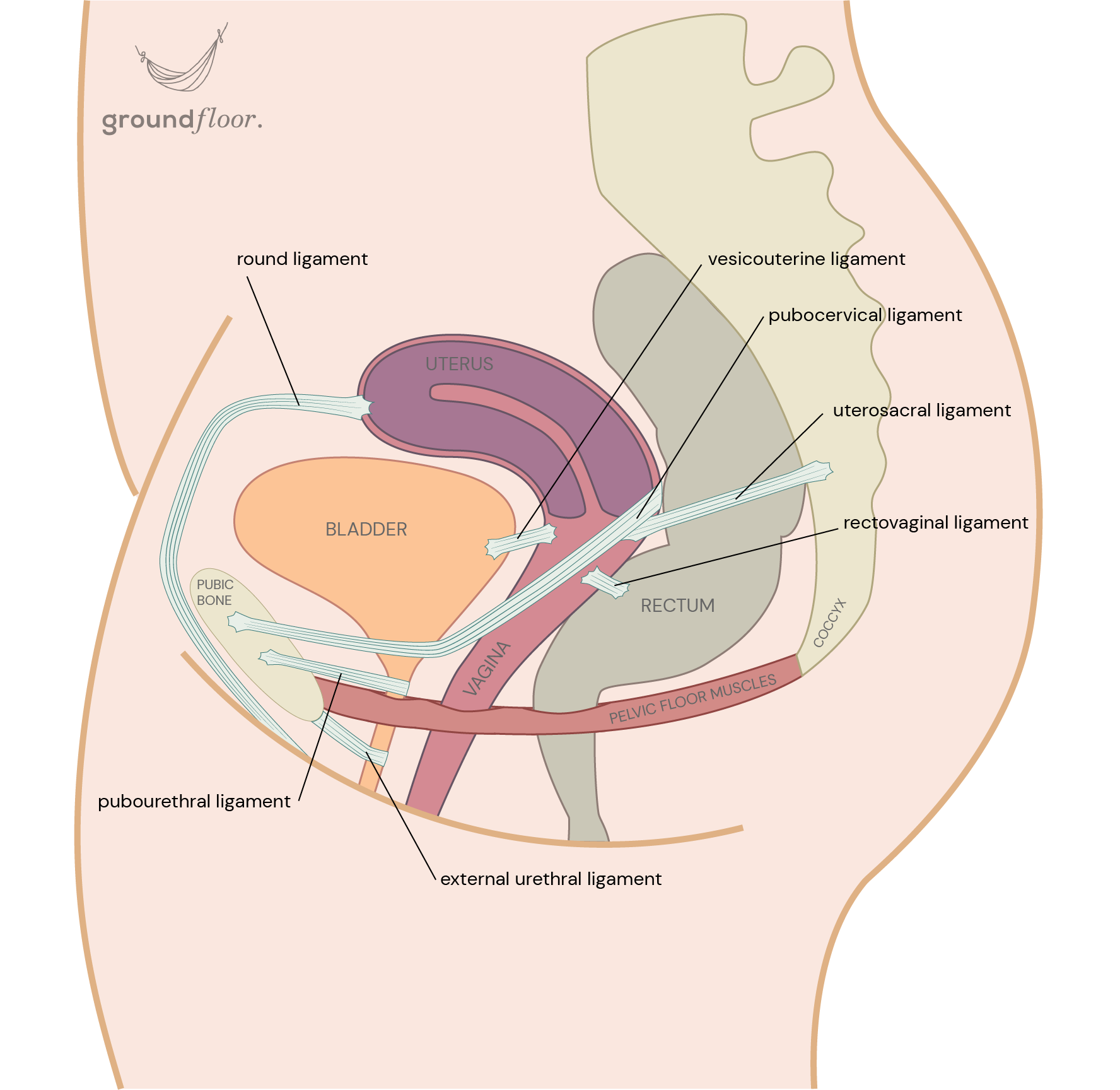
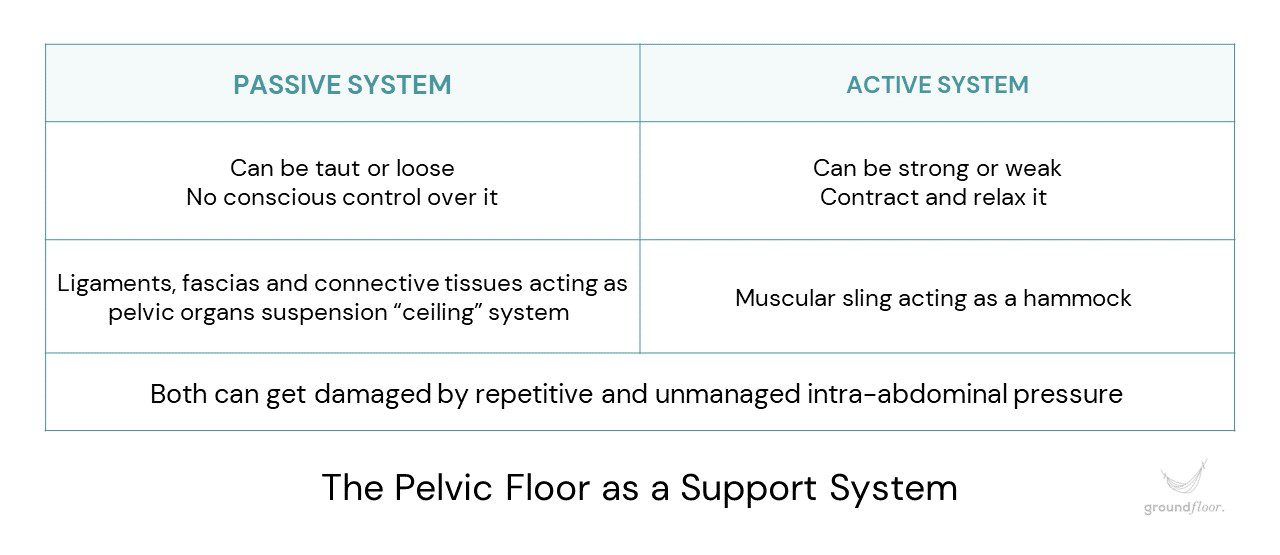
While the muscles uphold the pelvic contents from below, the ligaments, fascias, and connective tissues maintain it from above like a ceiling suspension system.
The consequences of a dysfunctional pelvic support
A pelvic floor that is weakened or injured is more prone to failing in its role of providing support, which can potentially result in a condition known as pelvic organ prolapse (POP), often referred to as organ descent. This involves the downward shifting of the bladder, uterus, or rectum from their usual positions. As a result, one or more of these organs may protrude into or through the vaginal area.
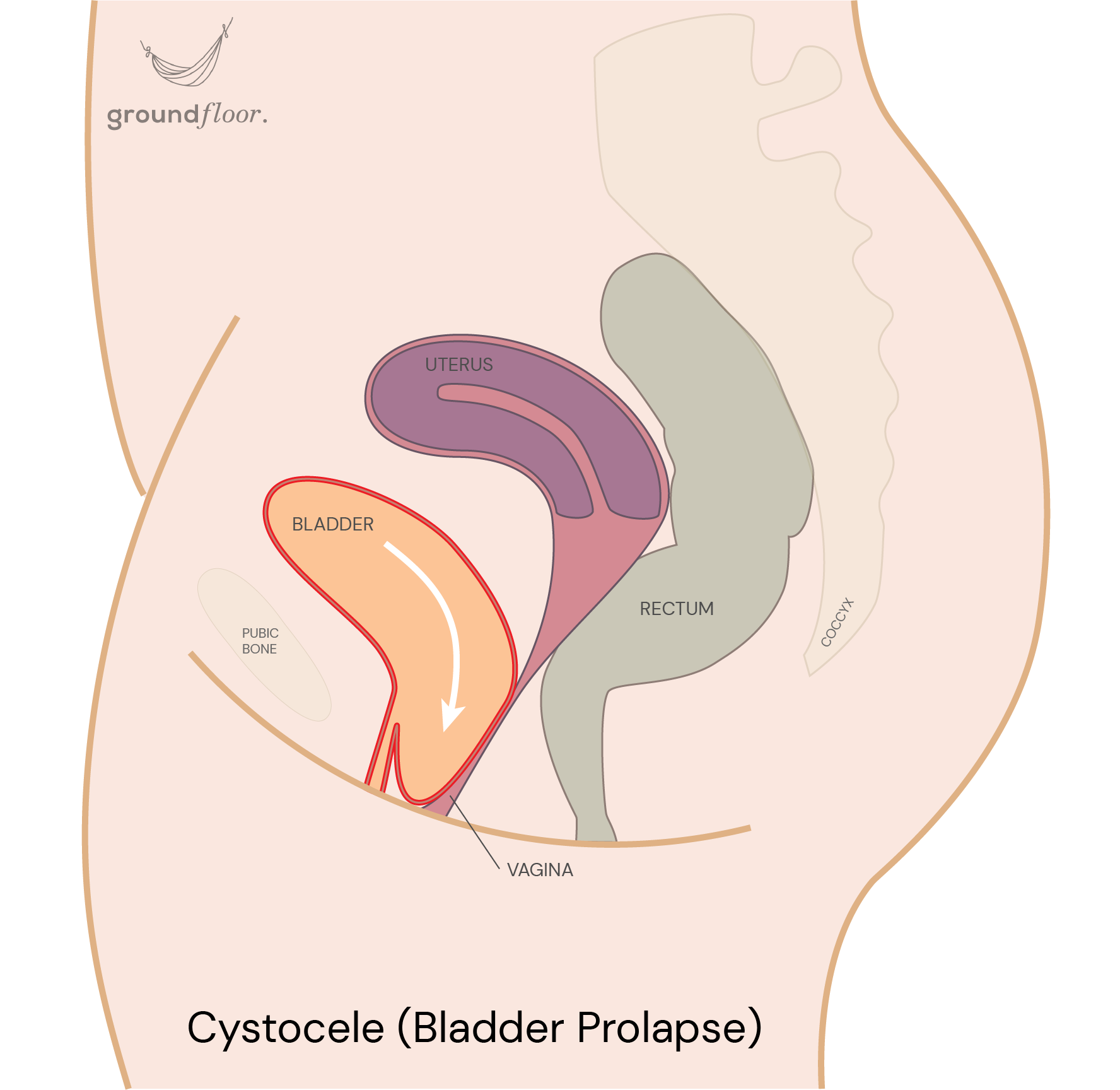
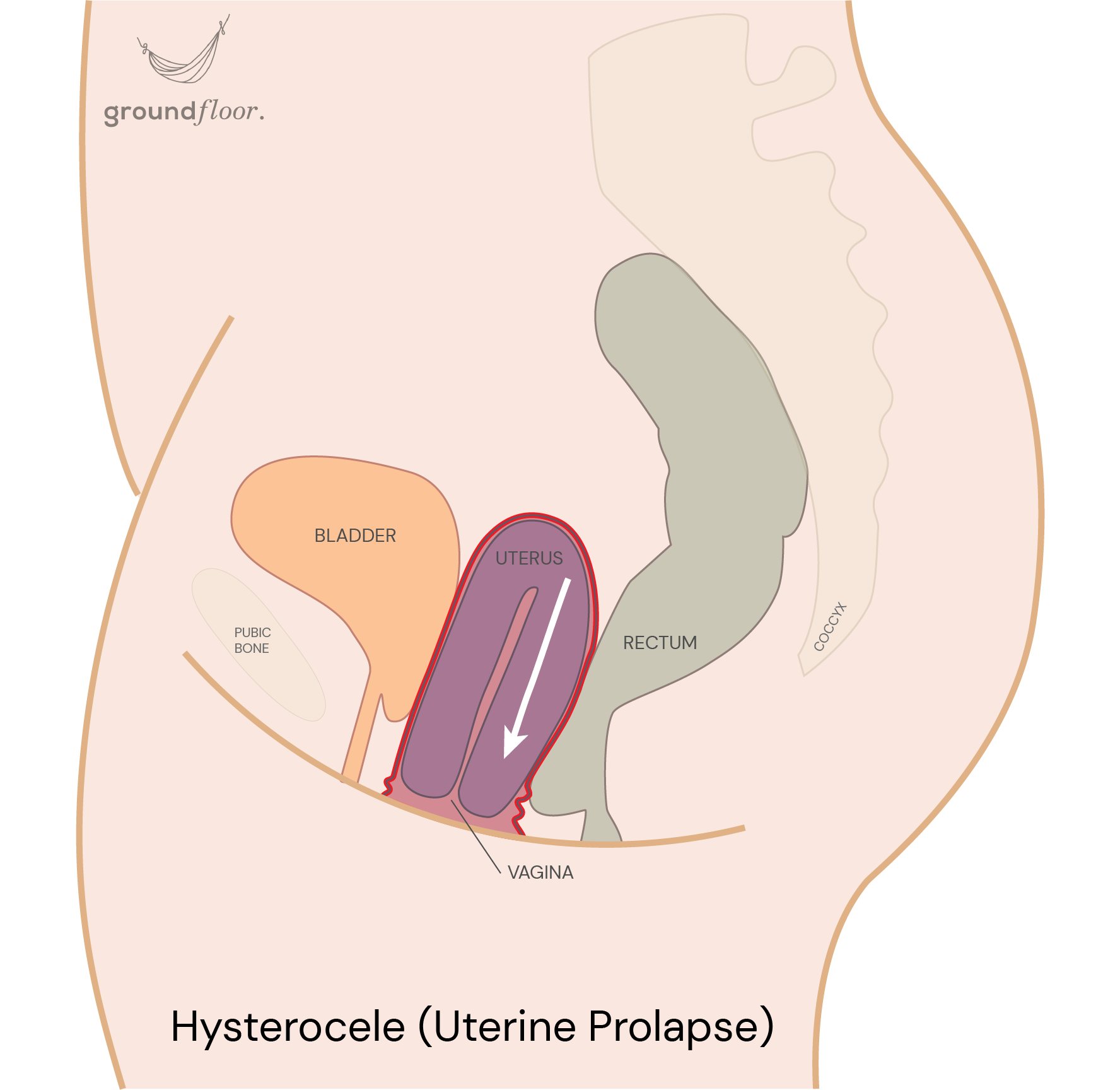
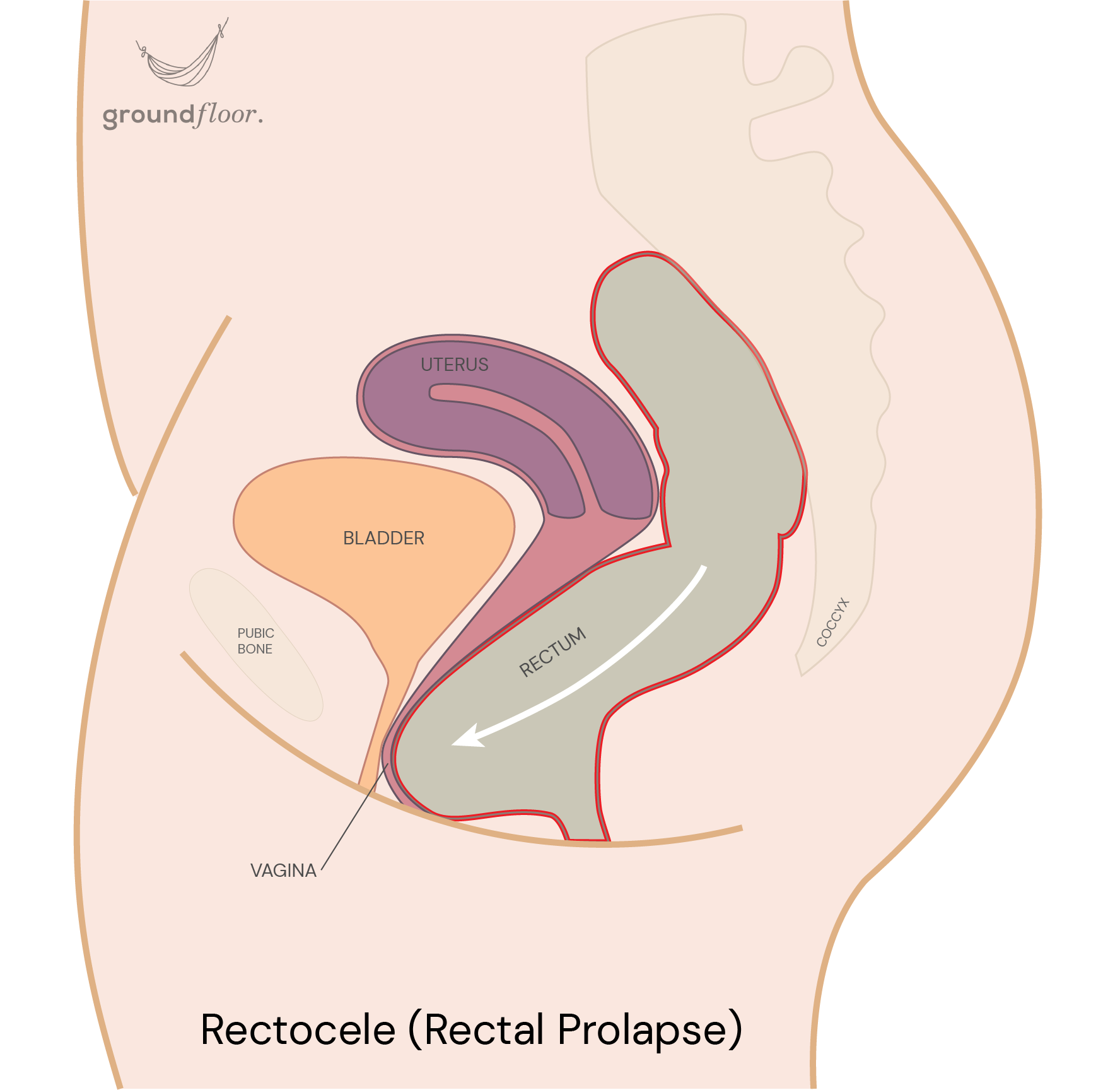
This condition varies in severity. Some cases are so mild that symptoms go unnoticed. In more severe instances, the affected organ might be entirely outside the vagina, requiring surgical intervention.This is why it is crucial to address a prolapse promptly to either reverse it or at least prevent its deterioration.
Our comprehensive pelvic health check-up is designed to identify a wide spectrum of symptoms or discomfort associated with pelvic organ prolapse, which may sometimes be overlooked by women.
In addition, perineal descent, also known as levator plate sagging, is a related condition often occurring alongside prolapse due to shared underlying causes. Unlike individual organ displacement, perineal descent involves a general shift of the pelvic contents as a whole. The perineum, situated between the vagina and anus and traversed by all pelvic floor muscles, loses its firmness and bulges downward, particularly during periods of strain. Consequently, the supportive pelvic floor "hammock" becomes loose, causing it to sag and balloon beneath the level of its attachment to the bone structure.
The role of a functional pelvic floor musculature for an effective support system
The singularity of the female anatomy lies in the presence of the vagina, which constitutes a structural gap within the pelvic floor muscles and creates a vulnerable area. Consequently, a functional musculature is imperative to maintain an effective support system for the pelvic contents. It prevents any shifting towards the void space of the vaginal canal and the occurrence of a prolapse.
When muscles experience weakening or damage (such as tears, episiotomies, or avulsions), their ability to contract and withstand downward pressure becomes compromised, elevating the risk of prolapse development. Notably, we find a higher number of organ descents in women with levator ani muscle injuries, as both contractility and resistance are impaired.
You can address the presence of prolapse or prevent its development with your tailored program. Ground Floor App provides targeted exercises designed to enhance the quality of the pelvic organs support system.
Protecting passive pelvic floor structures for effective support
Unfortunately, solely strengthening your pelvic floor is often insufficient to effectively address POP, given the multifaceted nature of its development. Indeed, the support function is not exclusively governed by the pelvic musculature. Ligaments, fascias, and connective tissues also play vital roles. They maintain the same tension without change and can't be voluntarily contracted or activated. They provide passive resistance against downward force, unlike your pelvic floor muscles, which offer an active and adaptive response against strain.
When these passive structures endure repetitive, excessive strain, they become lax, stretched, or damaged, thus losing their ability to hold the pelvic organs in place. The « suspension ceiling system » loses its tautness, which explains why we find lengthened and looser ligaments in women with prolapse.
Unfortunately, passive structures can't be directly strengthened, shortened, or tightened through exercises like your pelvic floor muscles can. However, you can protect them from becoming looser by managing the pressure within the abdominal cavity. Strategies to achieve this objective are detailed in the "Pelvic Floor Protection" guide.
It is also worth mentioning that, like any other tissues in your body, they can adapt over the long term with progressive load training. Nevertheless, it's crucial first to avoid adding undue stress, especially if the musculature isn't yet strong enough; otherwise, it could exacerbate organ descent and further damage the support system.
The consequences of intra-abdominal pressure on the support system
As the pelvic floor is subjected to forces coming from the trunk, repetitive strain along the years often causes alteration or damage to active and passive support structures. Indeed, poor pressure management within the abdominal cavity gets directly passed on to the pelvic contents. The leading causes are constipation, digestive issues leading to bloating, pregnancy, difficult childbirth, overweight, dysfunctional breathing patterns, core deficiency, etc. It can also result from hyperlaxity or a hormonal imbalance (like a reduction of estrogen level).
It is worth mentioning that the leading cause of pop development, excess downward pressure, is also a risk factor for incontinence. Unfortunately, one often comes with the other. Indeed, there is a correlation between both conditions. Up to 89,5% of women with prolapse also have some form of incontinence. The good news is that taking care of your pelvic floor and adopting healthy habits will target different issues simultaneously. You will benefit from your tailored program beyond your expectations!
In most cases, a comprehensive way to address pelvic organ prolapse entails learning to effectively manage intra-abdominal pressure along with pelvic floor strengthening. This approach prevents strain on the stabilizing structures and increases the level of support provided by the pelvic floor musculature.
However, it's worth noting that the lack of strength might not always be the root cause of the prolapse. In fact, an excessive level of muscle tone can also be an underlying factor.
The consequences of a hypertonic pelvic floor on the support system
A muscle characterized by excessive tension (known as hypertonic) can't correctly function and will struggle to stretch open for urine or bowel outflow. It leaves individuals with no recourse but to strain empty their bladder or bowels. Unfortunately, straining is a risk factor for prolapse development as it damages both the passive and active support systems.
Moreover, with an excess of tone, the pelvic floor lacks elasticity, inhibiting downward stretching. It hinders the ability to contract eccentrically, which is crucial in minimizing the forces exerted on the pelvic floor during an increase in intra-abdominal pressure.
Individuals with hypertonic muscles will usually benefit more from working on the ability to lengthen their pelvic floor instead of doing simple kegel exercises (repetitive concentric contractions only). In some cases, a combination of both is necessary!
If you want to know what your pelvic floor really needs, take the Check-up! It will ensure you don't lose your time, energy, and hope with an all-fit solution that would not be adapted to your situation and could potentially be detrimental to your pelvic health. With your tailored program, you have the opportunity to learn more about your body, tackle any existing concerns, and proactively prevent future issues.
Share this article with your friends and help spread the knowledge together! ↓
Share this article with your friends and help spread the knowledge together! →





Download the app to learn more about this topic and receive tailored information about your pelvic health!


Related articles
7 min read
The truth about having a tight pelvic floorA hypertonic or overactive pelvic floor (distinct from an overactive bladder) results from the buildup of excessive tension within the muscles. In this situation, the pelvic floor can also be referred to as "tight", which is often wrongly believed to be a good thing. This article will debunk this myth and shed light on the misconceptions surrounding this topic. Delving into the consequences of such a condition, we will also explore the common errors that can lead to a hypertonic pelvic floor and provide effective and practical strategies to address it.
→ Read more
3 min read
Turn on the automatic mode of your pelvic floorYou may have been training your pelvic floor wrong this whole time! One-size-fits-all exercises can't unlock the full potential of your pelvic floor. This article will discuss why tailoring your training is crucial to target your specific needs. You will also learn about the Knack, the alternative to doing Kegels forever, that will make your pelvic floor work automatically!
→ Read more
3 min read
Anatomy and functions of the pelvic floorToo many people have limited knowledge about the pelvic floor and its purpose, often associating it solely with urine leakage or childbirth. However, the truth is that the pelvic floor encompasses much more than that.
In this article, we will simplify the complex concepts of pelvic floor anatomy, functions, and mechanisms of action. Our goal is to make it easier for you to understand and appreciate the importance of this vital structure.
→ Read more

